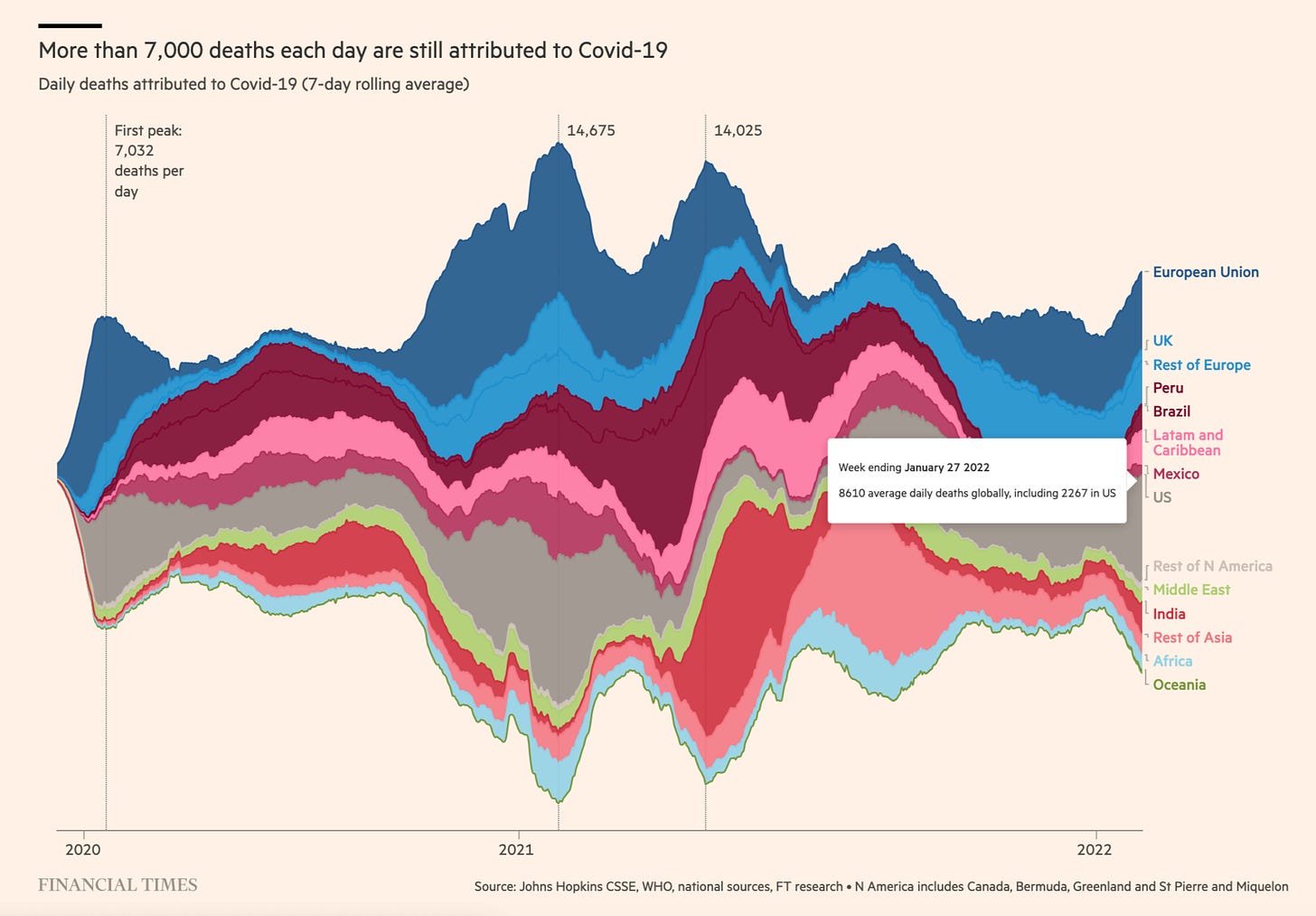
The @jburnmurdoch FT graph of COVID deaths is set to become the Minard-“1812”-graph of the COVID pandemic.
Source: FT
This is our reality folks. In the week ending January 27 2022, there were on average 8610 officially recognized COVID deaths per day, of which 2267 were in the USA. A similar number died across Europe (EU and non-EU). Those are staggering numbers.


As we debate whether the pandemic will soon be reclassified as endemic it is important to realize that this does not mean we are sounding the all-clear. As this excellent piece in Nature points out, smallpox was endemic until it was eradicated.
Meanwhile, this piece in the FT by Donato Paolo Mancini offers a useful roundup of efforts to put in place new mechanisms for ensuring more adequate responses in future.
In December, the World Health Assembly began debating a new pandemic preparedness treaty. Health Ministers from 30 countries signed an appeal in the BMJ for more serious preparation. It may yield an agreement ready for adoption by 2024.
As for our current situation, the big story for 2021 was the staggering success of the vaccine production drive. 11 billion vaccine doses were delivered in 2021, 1.5 billion in December 2021 alone. Production may double again to 20 billion in 2022. Of course, it would have been even better to have had more, even faster. But this is a prodigious feat of science and industry. The European Center for Disease Control estimates the lives saved among people over 60 years of age to be 470,000. For the US, the figure is 1.1 million.
The vaccines are crucial even if they are not 100 percent effective against Omicron-style variants.


But the tragedy is that costs, effectiveness and access vary hugely. The cost of the BioNTech/Pfizer gold standard is 20 euros per dose compared to 4 for AstraZeneca, which is the most widely used vaccine in the world, along with the Chinese Coronavac, with over 2 billion doses each.
And different costs are just part of the problem. The disaster, it is not too strong a word, is the gross maldistribution of vaccines.
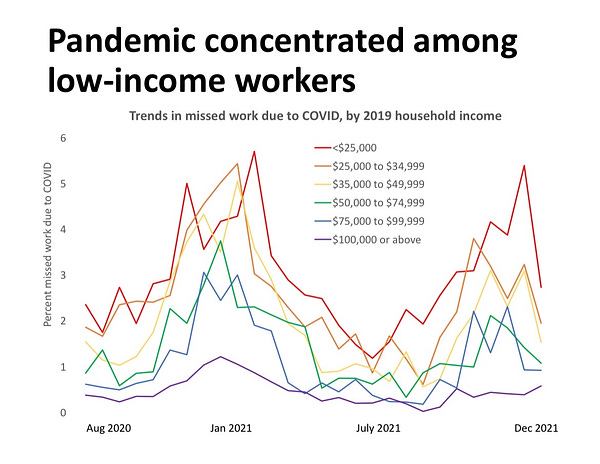
This takes three forms. Within rich countries, there is a continuing issue of the failure to protect lowest income workers. A complex issue with many factors at play.

There is a failure to deliver vaccines in a timely fashion to the most affected areas of the world. This includes the hot spots in Asia, Eastern Europe and Latin America.
Finally, there is the comprehensive failure to deliver very many vaccines at all to Africa. The continent is far from being the worst affected by the disease, but the failure to deliver vaccines is extraordinary.
Again and again the call has been made for comprehensive action. The most recent is this letter directed to the UK PM by a distinguished group of scientists. Reported on by the BBC.
COVAX was the designated vehicle for global vaccine delivery. Right now it is struggling to find funding for 2022. Gavi, its organizational backer, is hoping to raise an “ambitious” $5.2 billion to back its operations in the coming year. Right now it struggles to afford syringes.
As highly critical reports by the Bureau for Investigative Journalism and MSF have chronicled, COVAX was set up to fail. Failing to tie-in the main vaccine purchasing programs of the rich countries relegated it to the status of a second-class customer. And left it at the mercy of the rich-country producers.
It is a world away from the sort of amply funded urgent program envisioned by the IMF and experts advising the G20.
The disappointment of COVAX has meant that the world has relied more heavily on donations of vaccines than collective purchasing. Biden administration has made big promises. But those have, so far, resulted in an extremely patchy delivery. This gap is a feature of all donor commitments.
In the course of 2022 the absolute shortage of vaccines should end. It is estimated by March 2022 there should be a surplus of 1.4. billion doses in the US and Europe, enough to make real inroads on the African vaccination gap. But two questions must be put insistently. (1) Will the resources and organization be put in place to deliver the shots to the poorest billions of people worldwide? (2) Why, in a global medical emergency with gigantic economic costs, have the pace and terms of vaccine manufacture been set in such one-sided fashion by the manufacturers?
As investigative reports have established, Pfizer was unafraid to engage in brutal bargaining. Relations between Moderna and the Biden administration have been sticky too. Given Moderna’s heavy dependence on public funding, it is astonishing that the company should have any bargaining power whatsoever. It would not exist as a serious vaccine producer without public support of every kind.
With good reason profiteering from vaccine inequity has been denounced by Hassan, Yamey and Abbasi in the pages of the BMJ as a crime against humanity.
But, if individual companies that are beholden to public power and resources in so many ways are allowed to get away with this kind of behavior, this begs the question. Why are political figures not placing them under more serious pressure? Whatever technical and financial resources they may be able to muster, corporate power as we know it, does not exist independently of the state.
Here the brutal conclusion of one clear-eyed observer about the Biden administration:

At the global level , the commitment not to public command, but to lopsided public-private partnership runs deep in the lifeblood of Gavi, the parent organization of Covax. Even after the disappointments of 2021, Gavi boss Seth Berkley insisted to the FT that he remains committed to the partnership model and specifically the exclusive relationship between Oxford University, AstraZeneca and India’s Serum Institute. This was a relationship forged under the pressure of the Gates Foundation. And it is now widely seen as one of the main weaknesses of the COVAX construction. The higher-value deals with BioNTech/Pfizer and Moderna were left to the rich countries, whilst COVAX settled for contracts with India’s Serum Institute. It is a world-class facility but it is also the prime source of vaccines for the world’s second largest country that was itself suffering from a serious virus outbreak. Unsurprisingly, it turned out that the Serum Institute was not a reliable source of supply for the member countries of the COVAX initiative.
The failure by rich countries to adequately fund and supply a more generous and equitable global vaccination initiatives is commonly explained in terms of vaccine nationalism. But this is a superficial explanation that does not make sense in its own terms. Nature recently published a fascinating model that confirms the intuitive point that it is short-sighted and counterproductive for rich countries to hoard vaccines since the risk of virus mutation in unvaccinated populations leaves them vulnerable to new infectious strains.
A global vaccination campaign is NOT an act of charity on the part of rich countries. It is an act of enlightened self-interest. It is simply Realpolitik in the age of the anthropocene. As the IMF and every other competent agency have again and again pointed out, the benefits of ending the epidemic are, by any measure, orders of magnitudes larger than the costs of a global vaccination campaign.
The failure to devise more coherent and equitable vaccine production and distribution points not to a coherent national strategy so much as a vacuum of strategic vision and political panic, which lays governments open to strong-arm tactics by the likes of Pfizer. In 2018 Trump bullied Pfizer by tweet into retracting proposed price increases. In 2021 there was precious little bullying.
It is clearly true that purchasing the vaccine is just part of the cost of ultimate delivery. But there are carefully worked out models for the delivery of vaccines to even the most difficult territories. Take, for instance, this plan developed for the vaccination of South Sudan.
South Sudan aims to vaccinate 2,400,000 people by the end of 2021. Each vaccination team is 4 people and can vaccinate 80 people per day. That implies that each person on the team can vaccinate 20 people per day. • 20 people per day x 20 working days per month times 6 months = 2,400 doses of vaccine per worker. • To vaccinate 2,400,000 people within six months (or administer 4,800,000 doses of vaccine). That requires 2,000 members of vaccination teams working for 6 months. • An average salary for a health worker at this level is $300 per month. $300 x 2,000 people x 6 months = $3,600,000 Supervision and support for vaccinators: Additionally, each team and each county has a supervisor that supports the teams. There are also medical officers that provide support to teams. • Two team supervisor for every county = 158 team supervisors o Team supervisors get $450 per month o $450 x 158 supervisors x 6 months = $426,000 • One county supervisor for county = 79 county supervisors o County supervisors make $580 per month o $580 x 79 county supervisors x 6 months = $274,920 • One medical officer for every state = 10 medical officers o Medical officers make $580 per month o $580 x 10 medical officers x 6 months = $34,800 Total additional costs for supervisory and medical officer salaries = $736,320 Total costs. Total personnel costs = $4,336,320. $4,336,320 personnel costs divided by 4,800,000 doses = $0.90 per dose. Additional personnel costs are $0.90 per dose or $1.80 per person fully vaccinated.
The South Sudan model is based on online calculator for vaccination costs provided by the WHO.
Clearly, in the long-term, a far better model than charitably distributing vaccines would be for Africa, Latin America and poorer parts of Asia to produce and distribute their own vaccines. That would also allow local decision-makers to set their own priorities. As the FT reported:
during a recent meeting in Ghana, some of Africa’s public health leaders stated that “Covid vaccines are not our priority — we want malaria vaccines, we want vaccines which are for diseases that are causing high mortality in our countries.” Such concerns are underscored by data that show the collateral damage inflicted on wider public health goals by the pandemic — particularly in poorer nations. The WHO said last month that, of the 11 countries with the highest malaria burden, only India registered progress against the disease in 2020, as testing and the distribution of treatments were hampered by the Covid crisis. The 10 other countries, all in Africa, reported increases in malaria cases and deaths...
Malaria is one of the endemic killers with which African countries struggle. The news of the arrival of a Malaria vaccine is one of the highlights of 2021.
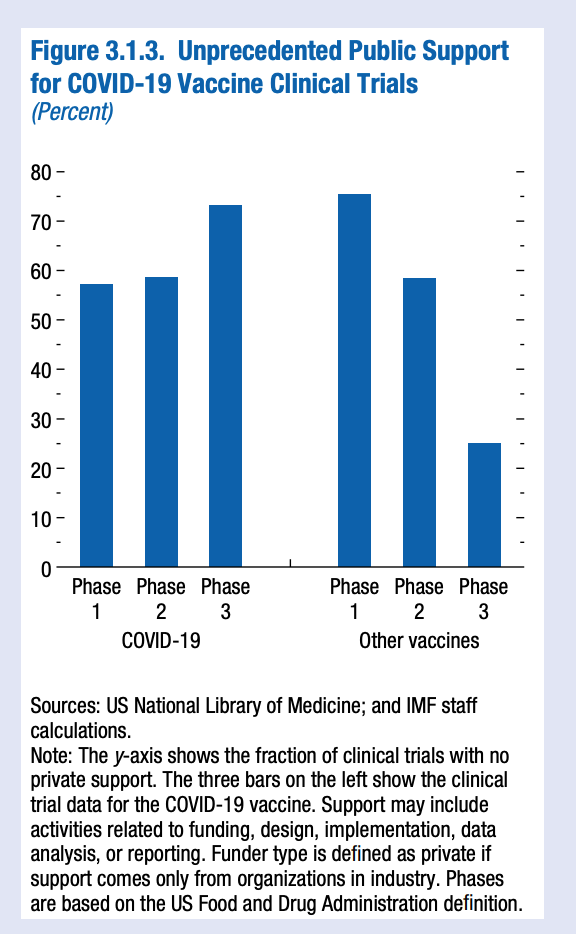
It has been decades in development. An overdue triumph of long-term commitment to public health research. Could it have come quicker? Surely yes, with the kind of funding and commitment received by the mRNA COVID vaccines in 2020. But for all their speed of development, they too profited from generations of scientific research. From the IMF came a particularly fascinating study of the successive layers of research that went into enabling the mRNA breakthroughs.
(mRNA) technology was built on waves of prior scientific discoveries. To track these discoveries, Figure 3.1.1 shows the publication dates of scientific articles cited by five of the seven Moderna COVID-19 vaccine patents (in blue).
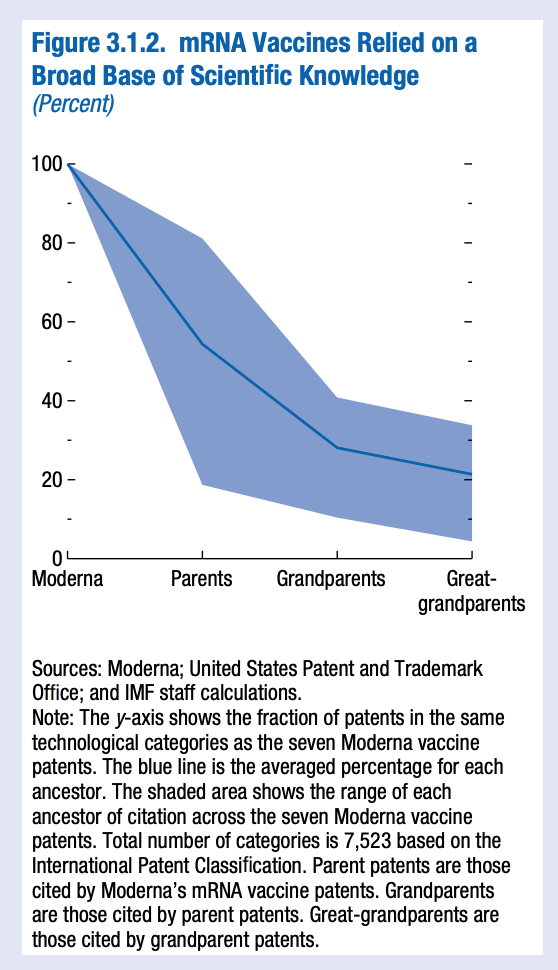
… To measure the indirect influence of science, the yellow line shows the scientific citations of the vaccine’s “parent” patents—other patents referenced in the five original vaccine patents. These peak in the early 2000s, tracking discoveries in editing genetic codes. Earlier advances in reading genetic codes drove a similar wave of citations from “grandparent” patents in the early 1990s. These waves of scientific influence illustrate how policies that help incentivize advances in basic science today influence the building blocks of future technologies and yield long-lasting economic payoffs. Developing mRNA vaccines relied on a broad base of scientific knowledge. On average, the Moderna vaccine patents are in the same technological category as only 55 percent of their parent patents—a number that falls further as citation chains lengthen (Figure 3.1.2).
This shows how wide-ranging basic science contributed to mRNA vaccines, indicating that policies to develop a broad scientific base can pay off in many and unexpected ways. The development of COVID-19 vaccines was encouraged by unprecedented public support. This included regulatory forbearance (emergency use authorization of COVID-19 vaccines), at-risk up-front investment and subsidies for vaccine production (Operation Warp Speed), help in scaling up manufacturing (Indian government grants to vaccine producers), joint licensing agreements with local producers (India, South Africa), and advance public purchase commitments (Israel, United Kingdom, United States). A distinguishing feature of public support for a COVID-19 vaccine was its continuation throughout the development process. Typically, public funding is most generous for early trials, falling as products near market. For COVID-19 vaccines, public and academic funding for clinical trials stayed high, even at the latest stages of development (Figure 3.1.3). This highlights how support throughout the production process can incentivize research by forward-looking firms.
This, obviously, should have major implications for future R&D expenditure and licensing agreements with private manufacturers of publicly-funded vaccines and medications. But, in 2022, there ought to be one simple priority. We will, finally, have enough vaccines. Get them in people’s arms, worldwide! There may be a minority that refuse. But we have no excuse for not providing vaccines to everyone who wants and needs them.
As Mike Ryan puts it:


***
I love putting out Chartbook. I am particularly pleased that it goes out for free to thousands of subscribers around the world. Voluntary subscriptions from paying subscribers support the effort. If you are enjoying the newsletter and would like to join the group of supporting subscribers, pick one of the options here.




Sometimes a snow needs to fall to see the tracks of the beasts: COVID certainly revealed the tracks of big pharma predators and how much real power they have as opposed to nominal power of regulators and "elected officials". In little over 10 years Pfizer went from example of biggest fraudsters in US corporate history (actually causing thousands of deaths), to "saviors" around which all government policies were wrapped up to give them monopolistic advantage.
https://www.justice.gov/opa/pr/justice-department-announces-largest-health-care-fraud-settlement-its-history
If I understand your discussion correctly, you seem to have provided more evidence of the state-corporate nexus being reversed: it seems that rather than states chartering corporations granting them certain rights and retaining the right to revoke their charter, now corporations rule the world, dictating to the state what the corporations will and will not do. This is especially egregious when taxpayer dollars are given to the corporation to fund the development of a product and then the corporation prices the product to generate 'excess' profits. Seems a lot like what Sheldon Wolin called Democracy, Inc.